




@Makeamom got me pregnant fast - I saved a ton doing it myself. I'm So Happy !
@Makeamom worked like nothing else. The cryobaby was perfect to use with our donor.
@Makeamom is the real deal. Their home insemination kit and fertility support supplements helped me go from years of struggling - To getting that Big Fat Positive on the test in my second month trying!
Before MakeAMom
You were guessing.
Tracking apps.
Timing everything perfectly, and still seeing one line.
Clinic visits felt expensive. Impersonal. Overwhelming.
You wanted this to feel hopeful… not stressful.


After MakeAMom
Now you feel prepared.
Confident. In control.
A simple, private at-home insemination kit — designed to support your fertile window
without the pressure of a clinic.
And when those two lines appear…
It feels intentional. Empowering. Yours.
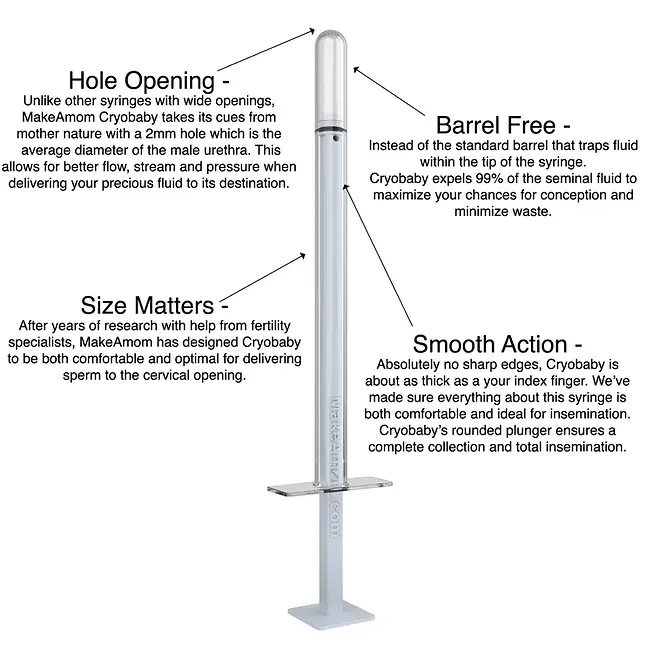
Designed to Support Your Journey
Privately & Confidently
💛 More Control Over Your Timing
Designed to help you inseminate during your most fertile window — without scheduling clinic appointments.
🏡 Completely Private
No waiting rooms. No awkward conversations. Just you, your partner, and your space.
💰 A More Affordable Option
Avoid thousands in clinical procedure costs while still taking a thoughtful, structured approach at home.
🧠 Clear, Step-By-Step Guidance
Straightforward instructions so you feel informed — not guessing.
🔄 Reusable & Thoughtfully Designed
High-quality components made for multiple cycles, helping you stay consistent without constant re-purchasing.
🌿 Made to Feel Personal — Not Clinical
Your fertility journey is intimate. Your tools should feel that way too.
Trusted by Thousands of Families Starting Their Journey
💬 Real Stories. Real Hope.

“After 6 months of trying, MakeAMom helped us feel like we finally had a plan. Two cycles later, two lines!”
— Jessica R.
“We weren’t ready for the cost of a clinic. This gave us a private, affordable first step.”
— Amanda & Chris
“The instructions were clear, the kit felt high quality, and most importantly it gave us confidence in the process.”
— Lauren M.
“It made something stressful feel assured.”
— Danielle S.
Why Families Trust MakeAMom
✔ Designed specifically for at-home intracervical insemination
✔ Thousands of kits shipped nationwide
✔ Discreet packaging & fast delivery
✔ Secure checkout & encrypted payment processing
✔ Responsive customer support

Backed by Research.
Built for Real Life.
Our approach is based on widely accepted intracervical insemination timing methods used in fertility care — adapted for at-home use in a way that feels approachable and empowering.





Still Have Questions? We Understand.
Starting your fertility journey is a big decision. Here are the most common concerns we hear — and how we address them.
💰 “Is this worth the cost?”
Clinic-based insemination procedures can cost thousands per cycle.
Many other at-home insemination options are single-use and disposable — meaning you repurchase everything each month.
MakeAMom is thoughtfully designed to be reusable, helping you stay consistent across multiple cycles without constantly starting over.
It’s a practical, cost-conscious first step for many families before considering more expensive interventions — while still supporting proper timing and technique.
⏳ “What if it takes time?”
Conception can take multiple cycles — even under ideal conditions.
Our kit is designed for consistency and repeat use, helping you stay prepared each month without starting from scratch.
Because success often comes from timing + persistence.
🧪 “Does at-home insemination actually work?”
Intracervical insemination is a widely recognized fertility method used in clinical settings.
MakeAMom adapts this approach for home use — empowering you with the right tools and guidance to support your natural fertile window.
Thousands of families have used this method as part of their journey.
🏡 “Is it complicated?”
Not at all.
Clear instructions.
Simple process.
Designed for privacy and ease.
No medical background required.
💛 “What if I’m nervous?”
That’s normal.
This is deeply personal.
MakeAMom was created to make the process feel:
-
Empowering instead of intimidating
-
Private instead of clinical
-
Hopeful instead of overwhelming


Thousands spent on single-use syringes, IVF and IUI.
MakeAmom is reusable.
Congratulations.
You’ve chosen a path to conception without tens of thousands lost to clinics or disposable solutions.
Not all at-home insemination options are the same.
Many are single-use, limited, or designed to be replaced again and again.
MakeAmom is different.
It’s a reusable system built to stay with you instead of charging you per attempt.
The video compares the leading devices on the market so you can see exactly where MakeAmom stands apart.

Need free sperm?
We got you covered -----> here
We Ship Our Home Insemination Kits to the US, UK, Canada, Australia, and World Wide.




_edited.jpg)
















